Merit-based Incentive Payment System
Quality Payment Program
How to Utilize This Manual
Please be aware: This document has been created solely for informational purposes and does not aim to confer rights or create obligations. The information included is merely a broad overview and is not designed to substitute for the actual laws, including associated regulations. We recommend that readers examine the relevant statutes, regulations, and other interpretive resources for a comprehensive and precise understanding of their contents.

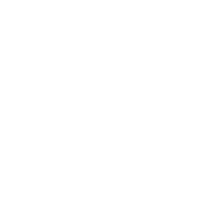
What is the Quality Payment Program?
The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) eliminated the Sustainable Growth Rate (SGR) formula, which was poised to cause considerable reductions in Medicare payment rates for healthcare providers. MACRA promotes a proactive, integrated approach for clinicians to effectively engage in the Quality Payment Program (QPP), which incentivizes value in one of two methods:
What is the Merit-based Incentive Payment System?

What is the Merit-based Incentive Payment System?
If you qualify for MIPS in 2024, the following requirements apply:
- You are required to report data on measures and activities related to the quality, improvement activities, and Promoting Interoperability performance categories.
- We will gather and compute data for the cost performance category on your behalf, if applicable.
- Your performance across the various MIPS performance categories, each assigned a specific weight, will culminate in a final MIPS score ranging from 0 to 100 points. • This final MIPS score will dictate whether you receive a negative, neutral, or positive adjustment to your MIPS payment.
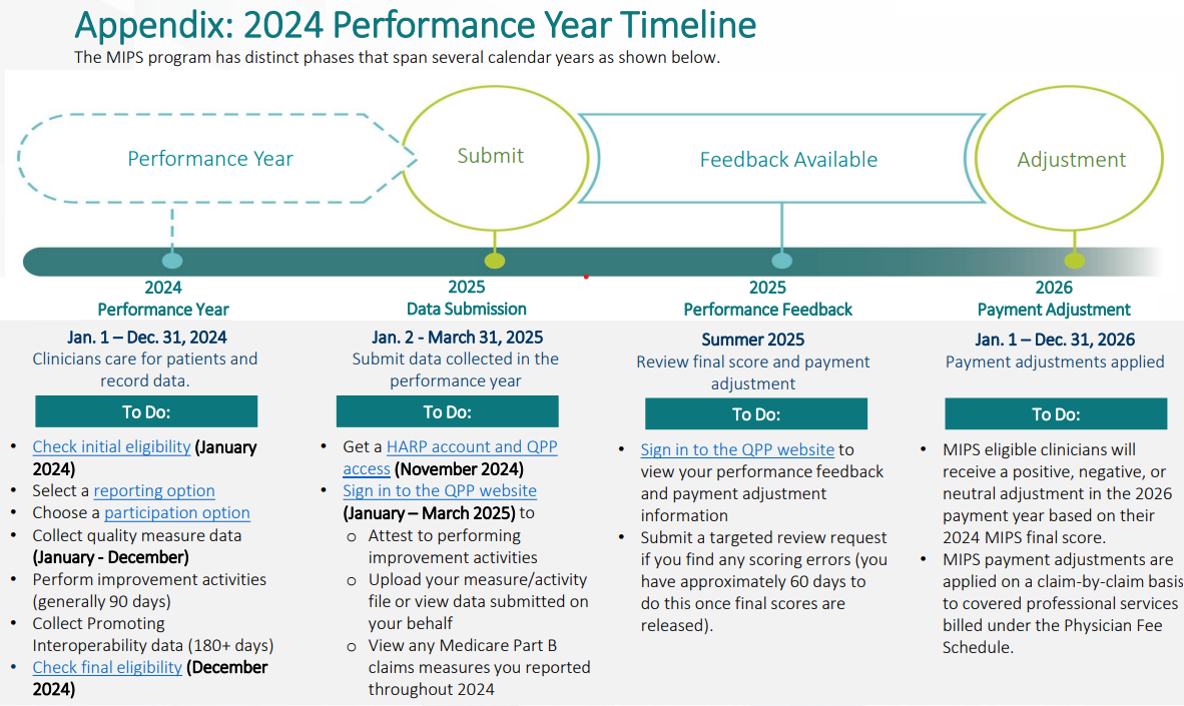
- The MIPS payment adjustment is contingent upon your performance during the 2024 performance year and will be reflected in payments for your Medicare Part B-covered professional services starting January 1, 2026.
Initiate Your Journey with MIPS in Six Steps
6 Steps for MIPS Participation in the 2024 Performance Year
Check Your Current Eligibility
Now
Select a Reporting Option
Now
Choose a Participation Option
Now
Select and Perform Your Measures and Activities
Throughout 2024
Verify Your Final Eligibility
Late 2024
Submit Your Data
Early 2025
What Occurs Following the Submission of My Data
A RCM company provides extensive support to U.S. healthcare organizations by supplying the personnel needed to process medical claims and submit them to insurance carriers for review and payment. We lead the industry in accomplishments, stability, and business excellence in key RCM services, including coding, charge posting, EOB/ERA posting, and accounts receivable management. Our experienced and seasoned team is capable of handling all specialties, offering 24/7 services to meet client service level agreements and quality standards.
Maintain Your Documentation (6 years)
Preserve records that substantiate the quality measures you have reported and the improvement activities you have undertaken. For further details regarding the suggested documentation for each improvement activity, please consult the 2024 MIPS Data Validation Criteria.
Examine Your Performance Feedback (Summer 2025)
Access the QPP website to assess your performance feedback. o Initial feedback can be accessed after the submission of data. o We expect that final scores will be published in mid-June 2025, with payment adjustment details available by mid-July 2025.
To access the preview of your 2025
MIPS performance data for public reporting, please log in to the QPP website. Examine Payment Adjustments (January 1 – December 31, 2026). Assess your claims to identify payment adjustments related to your 2024 performance, which will be applied individually to each claim for covered professional services billed in 2024.
Assistance and Edition History
Where Can Assistance Be Found
A RCM company provides extensive support to U.S. healthcare organizations by supplying the personnel needed to process medical claims and submit them to insurance carriers for review and payment. We lead the industry in accomplishments, stability, and business excellence in key RCM services, including coding, charge posting, EOB/ERA posting, and accounts receivable management. Our experienced and seasoned team is capable of handling all specialties, offering 24/7 services to meet client service level agreements and quality standards.
- To reach the Quality Payment Program Service Center, you may contact them via email at QPP@cms.hhs.gov, submit a ticket through the QPP Service Center, or call 1-866-288-8292 during business hours, which are Monday to Friday from 8 a.m. to 8 p.m. ET. For expedited assistance, it is advisable to call during off-peak times, specifically before 10 a.m. and after 2 p.m. ET. Individuals who are deaf or hard of hearing can connect with a TRS Communications Assistant by dialing 711.
- Explore the Quality Payment Program website for additional assistance and support information, to gain further insights into MIPS, and to access the resources offered in the Quality Payment Program Resource Library.
- Explore the Small Practices section of the Quality Payment Program website, where you can subscribe to the monthly QPP Small Practices Newsletter and access resources and information pertinent to small practices.
The Operation of MIPS Scoring
Each of the four categories assigns a score to providers, which are then added together to create the overall MIPS score. Higher scores indicate better performance, which is frequently possible with the help of MIPS consulting services. The MIPS score ranges from 0 to 100 points. Payment adjustments for the subsequent year are determined by the MIPS score. A positive payment adjustment, which entails greater compensation for services rendered to Medicare patients, is more likely to be granted to a provider with a higher score. On the other hand, subpar performance leads to lower reimbursement or negative payment adjustments.
Each category’s performance is given a score, which is subsequently weighted based on the previously mentioned percentages. A final score ranging from 0 to 100 is the resultant MIPS Composite Score, which is frequently supported by MIPS reporting services.
Methodical MIPS Composite Score Procedure
Category Scores
A provider’s performance in each of the four categories—quality, cost, improvement activities, promoting interoperability—is scored.
Weighted Average
Each category score is multiplied by its respective weight.
Composite Score
The weighted category scores are then added together to produce a final MIPS Composite Score.
Simplify MIPS 2025 Reporting with TechRcm
We at TechRcm are dedicated to giving healthcare providers the resources and assistance they require to thrive because we recognize how daunting the constantly shifting world of MIPS Consulting Services can be. Our all-inclusive, cloud-based practice management and EHR solutions are made to simplify MIPS reporting and assist you in: